NHLBI: Exploring Research Directions in Hope of a Widely Available Cure for Sickle Cell Disease
Style Magazine Newswire | 9/12/2017, 10:46 a.m.
September is not just “back-to-school” month; it’s National Sickle Cell Awareness Month—a month selected to call attention to a life-long illness affecting around 100,000 Americans, the majority of whom are African American or Hispanic.Sickle cell disease is accompanied by severe pain attacks and poor oxygen delivery throughout the body that can cause critical damage to organs. Currently, the only cure is hematopoietic stem cell transplantation (HSCT)—a costly procedure in which stem cells are taken from the bone marrow or blood of a healthy donor, and then injected into the recipient to generate red blood cells that do not sickle as do the cells in those with sickle cell disease—the characteristic that gives the disease its name. Unfortunately, many people with sickle cell disease in the United States don’t have a relative who is a full genetic match and able to be a donor.
The National Heart, Lung, and Blood Institute (NHLBI), a leader of federally funded research efforts on sickle cell disease, is actively exploring several safe and effective treatment options, and leading several initiatives designed to find a widely available cure for sickle cell disease. The institute supports many research efforts that yield new therapies, optimize current treatments, enhance pain management, and improve bone marrow transplant procedures to increase the body’s acceptance of donor stem cells.
One promising strategy that is being studied in a clinical trial – a study that tests how well a new medical approach works in people – is half-match bone marrow transplants. Bone marrow transplants can eliminate sickle cell disease, ridding them of painful and debilitating symptoms, and the need for a lifetime of pain medications and blood transfusions. This half-match approach could make bone marrow transplants accessible to more people living with sickle cell disease.
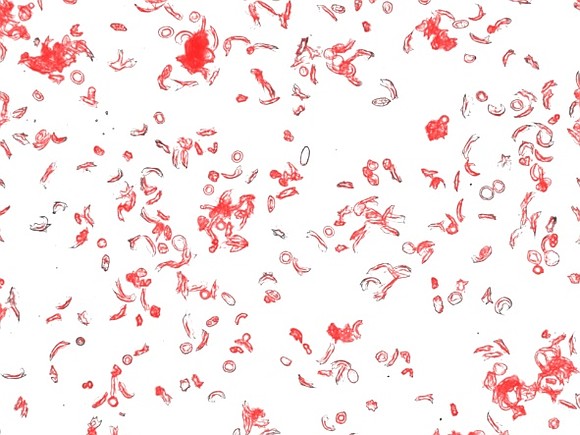
Mixture of normal and sickle-shaped red blood cells taken from a blood sample of a person with sickle cell anemia, as viewed through a fluorescent microscope. Image credit: Laurel Mendelsohn, Emilia Barbu, NHLBI The NHLBI also completed the Transcranial Doppler with Transfusions Changing to Hydroxyurea (TWiTCH) trial. Based on earlier research that was funded by NHLBI, regular blood transfusions have become the standard of care for reducing the risk of stroke in children with sickle cell disease. The TWiTCH study found that daily treatment with hydroxyurea— an oral medicine to help reduce or prevent several complications of sickle cell disease – is as effective as blood transfusions at reducing blood flow velocities in the brain, a key risk factor for stroke. NHLBI is committed to additional studies that can prevent strokes and other sickle cell-related complications.
Another area of promise for sickle cell disease treatment is gene editing, which involves changing the DNA. An NHLBI research group recently showed that correcting the sickle mutation in hematopoietic stem cells from patients with sickle cell disease, and then transplanting them in mice, resulted in enough normal hemoglobin to have a potential benefit. Another recent study in a patient showed that replacing the sickle mutation by gene insertion (gene therapy) resulted in complete clinical remission of sickle cell disease. However, longer follow-up in more patients is required to confirm the long-term safety and effectiveness of gene therapy for sickle cell disease.
NHLBI is also conducting early research using small molecule drugs. In one recent NHLBI-funded study, researchers found a small molecule that binds to hemoglobin and increases its ability to bind to oxygen; this could reduce sickling of red blood cells. Since small molecules can be easily administered, the hope is that this approach could become a cost-effective, widely available treatment for sickle cell disease both developed and developing countries. However, this approach has not been tested in humans yet.
Over the next decade, NHLBI is committed to conducting and funding innovative research on sickle cell disease. Sickle cell patients who participate in research studies are critical partners in discovering potential therapies and new approaches that improve our understanding of sickle cell disease. Although new preventive and treatment strategies might take years to develop, patients should take heart that today there are effective treatments that can help reduce symptoms and prolong life.
To find out more about how you or a loved one can participate in a clinical trial, go to clinicaltrials.gov and search sickle cell disease.