IVF Births Account for 2% of US Newborns: Here's What You Need to Know
Madeline Holcombe, CNN | 2/22/2024, 9:32 a.m.
Talk to a group of 100 people born in the United States, and chances are two of them were born as the result of in vitro fertilization, said Dr. Zev Williams, director of the Columbia University Fertility Center.
“In many ways, IVF is actually one of the great triumphs of modern medicine,” he said. “One thing that’s helpful to know is just how common it is. About 2% of births in the US results from IVF. Over 8 million babies have been born using this technology.”
Another technology important to the IVF process is cryopreservation of embryos — or freezing after the egg is fertilized.
The Alabama Supreme Court ruled Friday that frozen embryos are children and would be protected under the state’s Wrongful Death of a Minor Act.
As infertility experts warned about the impact on assisted reproduction, experts spoke to CNN to share what people should know about IVF and freezing eggs.
What is IVF?
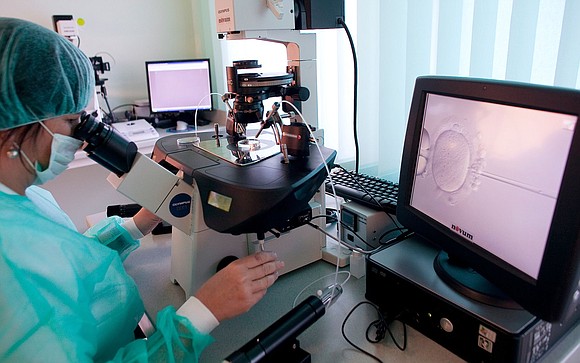
In vitro fertilization, or IVF, is when an egg is removed from a woman’s body and combined with sperm inside a laboratory before being implanted, said Dr. Eve Feinberg, associate professor of obstetrics and gynecology at Northwestern University’s Feinberg School of Medicine.
To accomplish that, patients undergo eight to 10 days of fertility injections with hormones that help their eggs mature, said Dr. Mamie McLean, an infertility specialist at Alabama Fertility in Birmingham. Egg retrieval procedures are done either in an outpatient or hospital setting and sometimes under conscious sedation, she added.
After fertilization, doctors watch the embryos as they develop, and what Feinberg often sees is that human reproduction is really inefficient, she said.
If 10 eggs are exposed to sperm, about seven will fertilize, she said. Of those seven, only 25% to 50% will grow in the laboratory long enough to be considered a more mature embryo called a blastocyst, Feinberg said.
From there, depending on the age of the patient, the blastocyst has between a 10% and 60% likelihood of becoming a baby, she said.
When is IVF helpful
IVF was first developed in the 1970s to help women with blocked fallopian tubes — the part of the reproductive system where sperm and egg meet, McLean said.
Since then, it has expanded to help conception in many other contexts, such as for people with recurrent miscarriages, male factor infertility, those utilizing surrogacy, and those for whom other fertility treatments have failed, she added.
“It’s our most successful treatment,” McLean said.
The technology has also allowed couples who carry genetic diseases to test their embryos and only transfer those that won’t be affected by those diseases, Williams said.
Why freeze embryos?
Freezing embryos is helpful for genetic testing, Feinberg said.
Clinicians take cell samples from the embryos to test them for genetic diseases or abnormalities, but it can take anywhere from two to four weeks for those tests to take place, she said. Freezing the eggs in the meantime keeps the eggs viable while health care providers look into genetic factors.
Patients can also choose to freeze embryos when they don’t intend to get pregnant right away, Feinberg said. Typically, there are higher success rates when fertilized embryos are frozen, not just the egg, she added.
Patients may choose to freeze embryos for medical reasons, such as before chemotherapy for cancer that may damage the ovaries. Or they can do it because they are not at the right stage of life to conceive but want to have a better chance at a pregnancy in the future, Feinberg said.
If one cycle of IVF can result in multiple embryos, freezing the embryos can keep those that were not implanted viable for future use, McLean said.
And whereas in the past, it was common to implant multiple embryos, freezing the embryos allows doctors to preserve the others for future use so one embryo can be implanted at a time — which is much safer for the patient and the future baby, Williams said.
Why not fertilize just one egg?
“It’s very much a numbers game,” said Dr. Serena Chen, advocacy director at CCRM Fertility in New Jersey and founder of Doctors for Fertility. “We are basically getting an entire year’s worth of eggs in one retrieval.”
The number of eggs is a large part of how IVF overcomes infertility, she added. Even in a young, healthy patient, about 30% to 50% of the eggs won’t develop into a pregnancy, Chen said.
“Just getting one egg at a time actually does not help improve the pregnancy rate, especially in somebody who’s infertile,” she said.
“The science behind IVF really shows that one single fertilized egg is not enough,” Feinberg said.
If her patients say they want two or three children, Feinberg encourages them to have between two to four embryos frozen for each, she said.
When a frozen embryo is warmed for implantation, there is about a 95% survival rate — meaning 5% won’t make it, Feinberg said.
Most patients will need at least two or three transfers before they become pregnant, McLean added.
Physicians now try to limit how many times they do egg retrieval and ovarian stimulation on a patient, because it does carry both health risks and a hefty cost, she said.
But families can choose to limit how many eggs are fertilized to create embryos, and before undergoing IVF, they talk with their doctor about their personal moral and ethical considerations, McLean said.
“All couples will make choices prior to going through IVF that relate to the disposition and use of their embryos,” she said. “These are patient-driven decisions that are the right choice for them.”



